Benefits and Drawbacks of Telehealth: Transforming the Provision of Healthcare
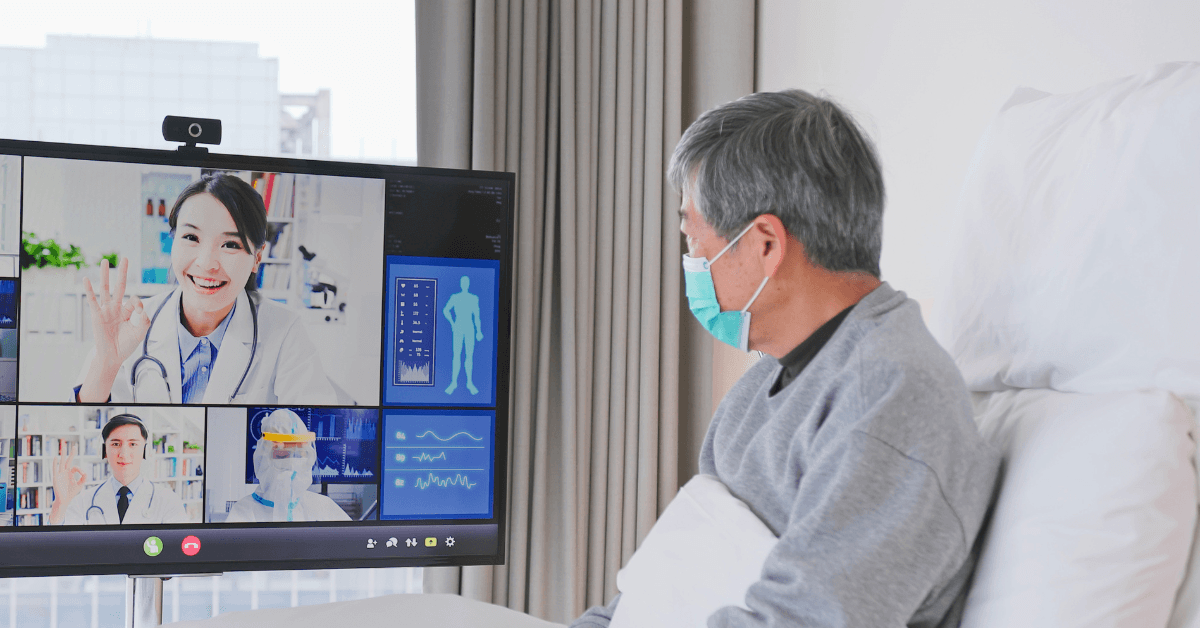
With the rapid evolution of the healthcare industry, telehealth has emerged as a transformative innovation. Telehealth Benefits and Barriers-Telehealth increases access to medical care by bringing patients and providers together digitally. Despite its numerous advantages, telehealth is not without its drawbacks. This blog offers insights into the changing role of telehealth in contemporary medicine by examining its main advantages and disadvantages.
The Growing Significance of Telemedicine-Telehealth Benefits and Barriers
Telehealth provides healthcare services online through the use of mobile apps, video conferencing, and remote monitoring. It was first implemented to alleviate the lack of healthcare in rural areas, but during the COVID-19 epidemic, its use exploded. Recent polls show that 82% of patients are now satisfied with virtual appointments. Telehealth is changing how medical professionals identify, treat, and interact with patients as technology advances.

Telehealth’s Main Advantages:
1. Improved Accessibility for Underserved Populations
Geographical obstacles are removed with telehealth, enabling patients in isolated or rural locations to visit professionals without having to travel. People with restricted mobility or limited access to transportation also gain a great deal. Additionally, busy professionals might cut down on time off work by scheduling appointments during breaks. Telehealth guarantees fair treatment for disadvantaged populations by democratizing access.
2. Patient and Provider Cost Savings
Virtual visits frequently save patients money on childcare, parking, and transportation compared to in-person sessions. Additionally, providers lower overhead costs associated with facility maintenance. Telehealth services are becoming more and more covered by insurance companies, which further reduces out-of-pocket expenses. As a result, households and healthcare systems are able to distribute resources more effectively.
3. Better Handling of Chronic Illnesses-Telehealth Benefits and Barriers
Through wearable technology and applications, telehealth makes it possible to continuously monitor diseases including diabetes, hypertension, and COPD. Real-time data is sent to doctors, enabling prompt treatment plan modifications. Readmissions to hospitals decrease as patients become more confident in their ability to manage their health. Frequent online check-ins encourage responsibility and guarantee sustained compliance with prescription drugs and lifestyle modifications.
4. Decreased Infectious Disease Exposure-Telehealth Benefits and Barriers
By reducing social interaction, virtual consultations shield immunocompromised patients from RSV, flu, and COVID-19. Online triage of non-urgent illnesses helps hospitals alleviate congestion as well. Additionally, telemedicine makes waiting rooms safer for both patients and workers by reducing the transmission of infections.
5. Anytime, Anywhere Support for Mental Health
Telehealth gives therapists and psychiatrists more freedom when treating PTSD, depression, and anxiety. By attending sessions from home, patients can escape stigma, and doctors can get to people in crisis more quickly. According to studies, teletherapy is a lifeline for millions of people, producing results that are on par with in-person appointments.
Obstacles to the adoption of telehealth-Telehealth Benefits and Barriers
1. Lack of connectivity and technology.
Access to telehealth is hampered by the fact that about 25% of rural Americans do not have dependable broadband. Disparities may worsen if older persons have trouble using cellphones or video platforms. Low-income households are unable to properly use services, especially in metropolitan locations, due to obsolete equipment and data costs.
2. Security and Privacy Issues
Concerns regarding data breaches during virtual visits have increased due to the rise in cyberattacks on healthcare systems. Despite the existence of HIPAA-compliant platforms, some patients are wary about using digital tools that handle sensitive data. To increase patient trust, providers should give staff training and encryption top priority.
3. Regulatory and Reimbursement Barriers
Patients and providers are confused by the significant variations in insurance reimbursement rules for telehealth. Certain jurisdictions limit access to out-of-state experts by prohibiting cross-border consultations. Regional variations in permanent legislation persist, notwithstanding the temporary COVID-19 flexibilities that were beneficial.
4. Physical Examination Restrictions
Telehealth is inadequate for illnesses like fractures or stomach discomfort that need physical examinations. Diagnostic mistakes might result from providers missing tiny visual clues. Although integration issues still exist, hybrid approaches that combine virtual and in-person care might lessen this problem.
5. Providers’ Opposition to Change
Due to workflow disturbances or a lack of experience with technology, many practitioners are hesitant to embrace telehealth. Incentives and training initiatives fall behind, overburdening providers. The promise of virtual care is undermined when burnout risks increase in the absence of institutional support.

Overcoming Obstacles in Telehealth
It takes teamwork to overcome these obstacles. Governments need to standardize reimbursement procedures and increase internet infrastructure. Healthcare companies ought to spend money on cybersecurity and user-friendly technologies. For telehealth to be implemented smoothly, providers must get continual training. By communicating their requirements and taking part in digital literacy initiatives, patients also contribute.
Telehealth’s Future
Telehealth, according to experts, will supplement traditional treatment rather than replace it. The majority of models will be hybrid, providing flexibility for regular examinations while saving in-person appointments for more complicated situations. 5G networks may make real-time remote operations possible, and artificial intelligence may improve diagnoses. Telehealth will probably become a vital component of patient-centered treatment as technology develops.
In conclusion
Unquestionably, telehealth has advantages such as increased access, cost reductions, and creative care delivery. However, issues like regulatory barriers and connection limitations need immediate response. Stakeholders can realize the full potential of telehealth and guarantee universal access to high-quality, egalitarian healthcare by removing these obstacles. In order to create healthier communities throughout the world, medicine must strike a balance between human competence and digital ease.
FAQ:
What are the benefits and limitations of telemedicine?
- Telemedicine facilitates chronic care, lowers expenses, and increases accessibility. However, there are drawbacks, such as privacy concerns, restricted physical examinations, and technological gaps. Making the switch to hybrid models can successfully handle these issues.
What are the barriers to telerehabilitation?
- Obstacles to telerehabilitation include uneven insurance coverage, a lack of hands-on therapy, and gaps in computer proficiency. Additionally, patients frequently lack equipment, and their level of participation declines in the absence of face-to-face encouragement, which hinders the rate of recovery.
Which benefits are most associated with the use of telehealth technologies?
- Telehealth facilitates real-time monitoring, increases accessibility in rural areas, and improves convenience. Furthermore, it improves mental health support and lowers infection exposure, resulting in timely and patient-centered care. High satisfaction ratings are highlighted by studies.
Who benefits from telehealth the most?
- Busy professionals, those with chronic illnesses, and people living in rural areas gain the most. Additionally, caregivers save time, and immunocompromised individuals have safer access to care. Its cost is especially essential for underprivileged urban populations.
What is the most significant reason that telehealth is important?
- By providing rural or vulnerable people with quick access, telehealth fills in care shortages. It saves lives by avoiding delays, particularly in times of crisis. Overall, it democratizes healthcare by emphasizing efficiency and equality.



