Overview
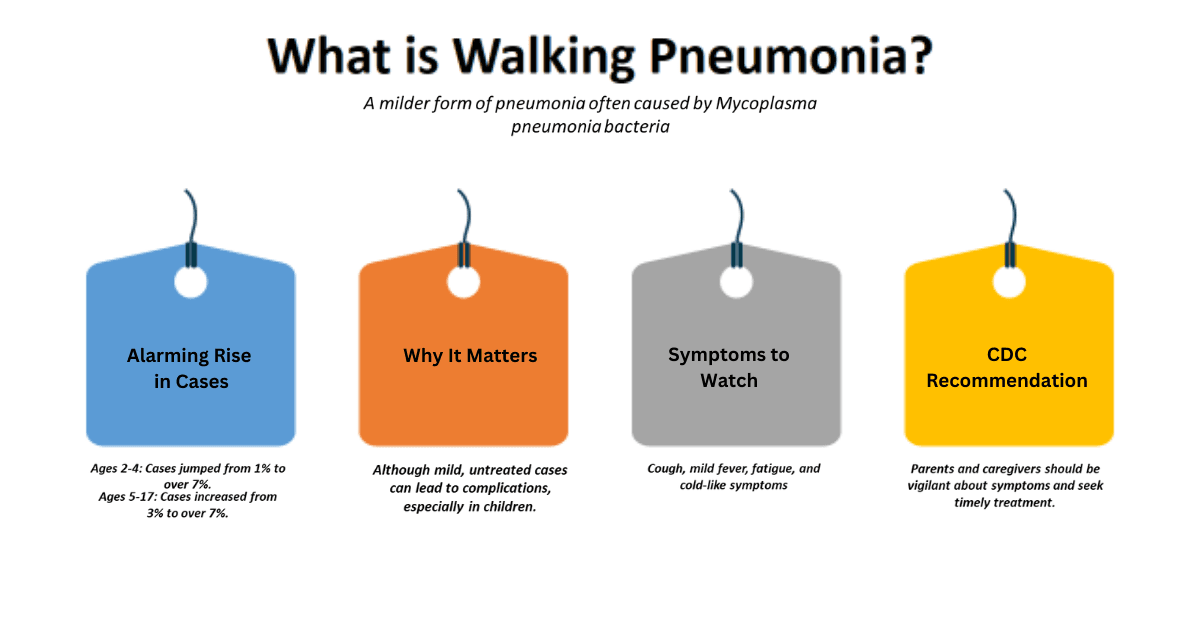
In the US, walking pneumonia—which is frequently disregarded since it is less severe—is becoming a serious health issue, especially for kids and teens. Rising Walking Pneumonia Cases Explained Health officials and parents should note the alarming increase in cases, which has increased from about 1% to over 7% in children aged 2 to 4 years and from about 3% to over 7% in older children aged 5 to 17. Recent reports from the Centers for Disease Control and Prevention (CDC) indicate that while walking pneumonia is typically less severe than traditional pneumonia, it can still lead to complications without treatment.
The recent increase in cases of walking pneumonia underscores the urgency of understandingThis rise can be attributed to a number of underlying factors. Healthcare professionals are emphasizing the importance of early diagnosis and appropriate management to mitigate the potential risks associated with untreated infections.
and recognizing this illness. Walking pneumonia, also known as atypical pneumonia, permits patients to carry on with their regular activities, in contrast to typical pneumonia, which frequently necessitates hospitalization. However, symptoms may vary from a persistent cough and exhaustion to a minor fever and chest pain. This particular case may lead many people to ignore their symptoms, potentially worsening the situation and contributing to the virus’s spread.
Walking pneumonia: what is it?
The bacterium Mycoplasma pneumoniae causes most walking pneumonia. Viruses or bacteria like Streptococcus pneumoniae cause the more common types of pneumonia. Walking pneumonia causes milder symptoms, including a persistent cough, headache, and weariness like the flu or cold. Because they can manage their symptoms at home and may not realize how terrible their situation is, people may continue their daily activities, unknowingly spreading the sickness.
It is particularly crucial to understand walking pneumonia during periods when its prevalence is at its highest. The less severe symptoms may conceal the underlying sickness, leading those afflicted to feel falsely secure. Furthermore, many parents may mistakenly believe that their child’s chronic cough is only a seasonal ailment, which could delay appropriate treatment and allow the germs to spread across communities.
What’s causing it to rise?
Several factors contribute to the startling increase in walking pneumonia cases this year. First of all, the tendency of respiratory viruses to overlap has grown alarming. Children are coming into contact with a variety of viruses as we return to more typical social contacts after the pandemic, which can make them more vulnerable to illnesses like walking pneumonia. This phenomenon particularly affects children who may not have previously encountered these viruses.
Increased pollution and changes in the environment can also impair immune responses, leaving people more susceptible to respiratory illnesses. The current climate fosters the spread of germs and viruses because of its variable temperatures and shifting weather patterns.
Lastly, there is a notable deficiency in immunity. Lockdowns and social distancing efforts during the COVID-19 epidemic have prevented many youngsters from experiencing natural exposure to a variety of illnesses. This lack of prior exposure has weakened herd immunity, facilitating the spread of illnesses among communities.
1. Comprehending walking pneumonia-Rising Walking Pneumonia Cases Explained
The Mycoplasma pneumoniae bacterium produces walking pneumonia, an unusual pneumonia subtype. Walking pneumonia has milder symptoms and different transmission properties than conventional pneumonia, which is often caused by viruses or Streptococcus pneumoniae. Small and cell-wall-less, Mycoplasma pneumoniae is a versatile bacterium that differs from other bacteria.
These bacteria can grow in the respiratory tract because they evade the immune system. Its small size and flexible cell wall allow it to infiltrate host cells more easily, making it more damaging. Walking pneumonia symptoms are often milder than bacterial pneumonia, delaying diagnosis and treatment. Many infected persons might continue their daily routines, increasing transmission risk.
Pathways of Transmission
When infected people cough or sneeze, respiratory droplets spread walking pneumonia. This transmission channel is especially concerning in close-quarters situations like workplaces, daycare facilities, and schools. Because the pathogen stays in the air for a long period, healthy people might breathe the virus without realizing it.
Due to the close proximity of children, diseases are more common in schools and daycare centers. Children may not wash their hands, share toys, or play together. Mycoplasma pneumoniae spreads easily in these environments, especially in winter when respiratory infections are widespread.
Walking pneumonia often has minimal symptoms, so infected persons may not realize they have it. Ignorance makes epidemics harder to manage because sick people continue their daily routines and unknowingly infect family, friends, and coworkers.
Symptoms
Walking pneumonia can have modest symptoms that are sometimes confused with the common cold or a moderate case of the flu, making prompt diagnosis more difficult. Typical signs and symptoms include:
- Fever: While typically less severe than the high fevers associated with normal pneumonia, a low-grade fever can occasionally occur.
- Painful Throat: Many people report having a scratchy or sore throat, which they sometimes mistake for a throat infection.
- Coughing: A common symptom that frequently becomes worse with time is a persistent, dry cough. Unlike the productive cough associated with more severe forms of the illness, the cough associated with walking pneumonia may not produce any symptoms.
- Weariness: People frequently experience generalized weariness, which leaves them feeling weak or listless.
- Headaches: Some people experience headaches due to their frequent association with various respiratory conditions, which can further complicate the diagnosis process.
Due to the slow development of these symptoms, people may disregard their illness as unimportant and delay seeking medical attention. Furthermore, people often mistake walking pneumonia for other respiratory illnesses due to its unusual appearance, underscoring the need for increased public and healthcare practitioner awareness and comprehension.
Similarity to Common Pneumonia-Rising Walking Pneumonia Cases Explained
Walking pneumonia often progresses more slowly than ordinary pneumonia, which is characterized by a rapid start and more severe symptoms including chills, a high fever, and a productive cough with phlegm. This slow rise may lead patients to believe they are simply experiencing a seasonal cold. Even in less severe cases, one should not ignore walking pneumonia. In susceptible groups like small children and older people, it might result in problems like ear infections or bronchitis if treatment is not received.
Growing Awareness and Cases
Recent CDC studies show a rise in children’s walking pneumonia. The incidence has grown from 1% to over 7% in toddlers aged 2–4 and from 3% to over 7% in older children aged 5–17. Health professionals have stressed vigilance and early action in response to this spike.
Cases are rising for several reasons. First, the convergence of respiratory infections makes youngsters more susceptible to walking pneumonia. After the outbreak, children continue their typical social connections and encounter more diseases, which may impair their immune systems.
Seasonal changes and pollutants can also weaken immune responses, making respiratory diseases more likely. Uneven weather helps Mycoplasma pneumoniae spread easier.
Finally, prior pandemic constraints have restricted the exposure of many children to common illnesses. This lack of exposure has lowered herd immunity, making walking pneumonia more likely to spread throughout communities.
2. Reasons for the Increase-Rising Walking Pneumonia Cases Explained
Both parents and health officials are concerned about the recent spike in walking pneumonia infections, especially in young children. We can blame this phenomenon on numerous interconnected elements that have surfaced in the post-pandemic environment. In this blog post, we will explore the potential causes of this increase, the impact of air quality and climate on respiratory infections, and the response from the medical community.
Possible Reasons
1. Gaps in Post-Pandemic Immunity-Rising Walking Pneumonia Cases Explained
Walking pneumonia has increased due to the COVID-19 pandemic immunity gap. Lockdowns prevented many children from getting common childhood illnesses, including Mycoplasma pneumoniae, which causes walking pneumonia. When children returned to school and social life, their immune systems encountered these germs again, causing respiratory infections.
The outbreak also reduced standard vaccines and health checks. This lowering puts many kids at risk for diseases they would normally be immune against. Recently reported increases in walking pneumonia cases show the impact of immunity gaps.
Delayed Medical Care
Another reason walking pneumonia has increased is people’s delayed healthcare access during the pandemic. Since COVID-19 was the priority, hospitals and clinics overlooked non-COVID disorders. Fearing viral exposure, many parents avoided medical treatment for their children’s respiratory issues. Walking pneumonia, typically neglected early on, became more severe due to this delay in diagnosis and treatment.
Mental health impacts of the epidemic are unavoidable. Some parents may have skipped their kids’ normal doctor’s appointments out of concern for their health. Due to untreated infections that become walking pneumonia, incidence rose dramatically.
Seasol factors also strongly influence walking pneumonia. Fall and winter respiratory diseases rise due to decreased weather, increased indoor time, and seasonal viruses. Walking pneumonia is more likely when these seasonal factors mix with children’s heightened vulnerability owing to immunity gaps and healthcare delays.
Air quality and climate-Rising Walking Pneumonia Cases Explained
The quality of the air in cities has a big influence on respiratory health. Excessive air pollution, including industrial pollutants and vehicle particulate matter, can make respiratory diseases worse. The negative effects of air pollution can damage children’s respiratory systems and increase their susceptibility to diseases like walking pneumonia. This is especially true for children who live in urban areas.
Research has linked poor air quality to respiratory diseases, including pneumonia. The risk of respiratory symptoms, such as coughing and trouble breathing, rises with declining air quality, making the environment unpleasant for kids who already have respiratory disorders.
2. Seasonal Variations
Seasonal variations can also affect the prevalence of respiratory illnesses. For example, respiratory infections may be more likely to survive and spread in colder climates. Wintertime brings more people together inside, which makes it easier for germs like Mycoplasma pneumoniae to spread among kids. This trend of higher transmission throughout the winter months emphasizes the need for heightened attention to respiratory health during these times.
The Reaction of the Medical Community-Rising Walking Pneumonia Cases Explained
1. Enhanced Awareness Initiatives
The CDC and regional health organizations are increasing awareness programs targeting parents and caregivers in response to the increase in walking pneumonia cases. The goal of these programs is to inform families about walking pneumonia’s symptoms, which are frequently mild and confused with the common cold. Parents should seek medical assistance if their child exhibits symptoms including a moderate temperature, exhaustion, or a persistent cough.
Additionally, medical professionals should emphasize the importance of regular, periodic checkups for children. Health officials want to close these gaps in order to lower the prevalence of respiratory infections and enhance children’s overall health outcomes.
2. Endorsing preventive actions
Additionally, local health organizations are taking precautions against the effects of respiratory illnesses. This involves promoting improved air quality by changing laws to lessen pollution and enhance urban planning. Furthermore, we are urging schools to implement health policies that support respiratory hygiene, including promoting mask use and hand washing during periods of high infection.
Healthcare professionals are now being asked to take a more proactive approach to diagnosis and treatment, which includes educating parents and kids about identifying early signs and getting medical attention quickly to avoid consequences.
3. We are comparing walking pneumonia with other respiratory conditions.
Comparative Evaluation: Recognizing the Disparities-Rising Walking Pneumonia Cases Explained
Walking pneumonia, often referred to as atypical pneumonia, is a less severe kind of pneumonia that is mostly brought on by certain bacteria, such as Mycoplasma pneumoniae; however, viral infections can also cause it. In contrast to typical respiratory ailments like bronchitis and seasonal flu, as well as classical pneumonia, this disorder exhibits unique symptoms.
1. Comparing Walking Pneumonia with Conventional Pneumonia
Usually brought on by viruses like influenza or bacteria like Streptococcus pneumoniae, regular pneumonia is typically more severe. Hospitalization is frequently the result of typical pneumonia symptoms, which include a high temperature, a severe cough, and chest discomfort. Patients with walking pneumonia, on the other hand, are less likely to recognize that they have the illness since their symptoms are milder. The phrase “walking” pneumonia refers to the fact that patients frequently carry on with their regular activities. People often confuse its symptoms, such as a low temperature, headache, exhaustion, and a persistent dry cough, with those of other respiratory disorders.
2. Comparing bronchitis with walking pneumonia-Rising Walking Pneumonia Cases Explained
A productive cough that generates mucus is a common symptom of bronchitis, an inflammation of the bronchial tubes. Acute bronchitis typically follows a viral illness like the flu or a cold. A cough is a common symptom of both walking pneumonia and bronchitis, although walking pneumonia typically has a less productive cough that lasts for several weeks. Furthermore, walking pneumonia may persist longer and require antibiotic therapy, whereas bronchitis symptoms may improve quickly.
3. Draw a comparison between seasonal flu and walking pneumonia.
The influenza virus, which causes the seasonal flu, frequently manifests as high fever, chills, body aches, and exhaustion. Flu symptoms can be abrupt and incapacitating, causing substantial downtime, in contrast to the milder walking pneumonia symptoms. While coughing and exhaustion are frequent symptoms of both illnesses, systemic symptoms are more prevalent in the flu and less common in walking pneumonia.
Particular features of walking pneumonia-Rising Walking Pneumonia Cases Explained
Walking pneumonia differs from other respiratory diseases in a number of ways, especially in terms of symptoms, contagiousness, and demographic spread.
1.Light Symptoms
Walking pneumonia is characterized by its mild symptoms. A low-grade fever, sore throat, exhaustion, and a chronic dry cough are possible symptoms for patients. In contrast to ordinary pneumonia, these symptoms frequently do not render the patient incapacitated, enabling them to continue with their normal activities. Since many people choose not to seek medical attention when their symptoms are moderate, this mildness may result in underdiagnosis.
2.Contagiousness
Respiratory droplets are the primary means of transmitting walking pneumonia when an infected individual coughs or sneezes. Because people with walking pneumonia may readily spread the virus to others, especially in crowded settings like workplaces and schools, this feature makes it more like the flu than ordinary pneumonia. Walking pneumonia is not as virulent as more severe forms of the illness, despite its infectious nature.
3. Distribution of Demographics-Rising Walking Pneumonia Cases Explained
Children and young adults are more likely than older persons to get walking pneumonia. Younger people frequently come into close contact with one another, particularly in school environments where respiratory diseases can spread quickly, which is why this demographic is more likely to get walking pneumonia. Furthermore, many young people are particularly vulnerable because they have not yet developed immunity to the bacteria that cause walking pneumonia.
Recognizing Risk Elements-Rising Walking Pneumonia Cases Explained
Walking pneumonia can occur as a result of a number of risk factors. Age, the environment, and the state of the immune system are all important factors.
- Age: As previously shown, young adults and children are more vulnerable. But people with compromised immune systems or those over 65 are also at risk.
- Environmental Conditions: The bacterium that causes walking pneumonia can spread more easily in crowded living situations, especially in metropolitan areas. Exposure to tobacco smoke and poor air quality might worsen respiratory conditions.
- Immune System Status: People who have weakened immune systems, whether as a result of long-term medical conditions or drugs, are more susceptible to walking pneumonia.
Intervention and avoidance.
- Even though walking pneumonia is often mild and goes away on its own, some severe instances may require antibiotics. Since macrolide medicines like azithromycin and clarithromycin work well against the bacteria that most frequently cause this illness, doctors usually prescribe them.
Preventive interventions are crucial in lowering the prevalence of walking pneumonia.
- Vaccination: Maintaining current immunizations, such as the flu shot, might help shield people from conditions that could make them more susceptible to walking pneumonia.
- Good hygiene practices: Routine hand washing, avoiding close contact with sick people, and practicing respiratory hygiene, which includes covering the mouth and nose when coughing or sneezing, can reduce the transmission of the germs.
- Healthy lifestyle choices: Maintaining a robust immune system through a proper diet, consistent exercise, and adequate sleep can prevent respiratory infections.
4. Current data and patterns-Rising Walking Pneumonia Cases Explained
Recent Surge Statistics
There has been a worrying increase in “walking pneumonia,” especially in youngsters in the US, according to recent research. The bacteria Mycoplasma pneumoniae frequently causes walking pneumonia, which many people underestimate due to its milder symptoms compared to regular pneumonia. The CDC reports that there has been an extraordinary increase in cases of this virus, particularly in young children between the ages of 2 and 4, underscoring the urgent need for education and preventative actions in this susceptible age range.
In actuality, pneumonia kills more than 700,000 children a year, or over 2,000 per day, making it the most common infectious disease-related cause of death for children under five. This sobering fact emphasizes how urgent it is to treat pneumonia cases, especially walking pneumonia, which has become more common recently.
Regional Information-Rising Walking Pneumonia Cases Explained
Regional data reveals a higher incidence of walking pneumonia cases in some states. For instance, the CDC has noted a higher number of recorded incidents in areas such as metropolitan centers with high densities of young children. The CDC has identified Texas and California as particularly impacted states. Medical professionals in these regions are more vigilant in identifying and disclosing respiratory diseases, which may account for the observed increases.
Additionally, a major contributing factor to the occurrence of walking pneumonia is the seasonality of respiratory illnesses. Cases tend to increase as fall approaches because more people are congregating indoors, which makes it easier for the bacterium to spread. Parents and guardians should monitor for symptoms of walking pneumonia, such as fatigue, a moderate temperature, and a persistent cough.
Global Viewpoint
Global trends for walking pneumonia are concerning yet consistent. Several nations are witnessing similar increases. For instance, recent reports from the UK show an increase in Mycoplasma pneumoniae infections, especially in children, which is similar to what is happening in the U.S. This implies that the factors causing the increase in walking pneumonia might be a part of a larger pattern, perhaps connected to changes in climate and social behavior that affect the spread of respiratory infections.
The United States has achieved progress in immunization and health education compared to other countries, which has typically contributed to a decrease in severe pneumonia cases. But the development of walking pneumonia poses a special difficulty. Reports of growth in antibiotic-resistant forms of Mycoplasma pneumoniae in nations like Australia have raised concerns over the efficacy of existing treatment regimens.

5. Options for diagnosis and treatment-Rising Walking Pneumonia Cases Explained
Methods of Diagnosis
Doctors use a variety of clinical evaluations and diagnostic instruments to diagnose walking pneumonia, particularly when Mycoplasma pneumoniae is the cause. A comprehensive physical examination is usually the first step in the procedure, during which a medical professional assesses the patient’s medical history and current symptoms. Using a stethoscope, the doctor will listen to the lungs during this examination in order to detect any unusual breath sounds, such as crackling or wheezing, which may be signs of fluid or inflammation in the lungs.
X-rays of the chest are a common diagnostic technique in addition to the physical examination. This imaging method allows for the visualization of the lungs and enables the detection of any anomalies, including regions of consolidation resembling pneumonia. Lab tests are the next step in the diagnostic process since, although chest X-rays can confirm the existence of pneumonia, they are unable to identify the exact causative pathogen.
Identification of Mycoplasma pneumoniae is mostly dependent on laboratory testing. A medical professional may prescribe a sputum culture, which involves taking a sample of lung mucus and examining it for bacteria. However, other tests like PCR testing, which identify bacterial DNA, or serological tests, which identify antibodies against the germs, may be used for a more accurate diagnosis because Mycoplasma pneumoniae can be difficult to cultivate. In situations where the patient is displaying severe symptoms, we may conduct additional tests, such as blood testing, to assess general health and the presence of infection.
Options for treatment-Rising Walking Pneumonia Cases Explained
Following confirmation of the diagnosis, walking pneumonia is usually treated with a mix of medicines and symptomatic treatments. In order to treat bacterial pneumonia, antibiotics are necessary. Particularly for walking pneumonia, doctors frequently prescribe macrolides like azithromycin and clarithromycin due to their efficiency against Mycoplasma pneumoniae. Doctors may occasionally suggest tetracyclines or fluoroquinolones, especially for older individuals or those with specific medical issues.
Doctors frequently recommend patients take over-the-counter (OTC) drugs in addition to antibiotics to relieve their symptoms. Acetaminophen and ibuprofen are examples of pain medications that can help lower fever and ease body aches. We may also recommend expectorants and cough suppressants to treat a persistent cough and promote better relaxation and recuperation. Patients must follow their healthcare provider’s advice about drug doses and treatment duration to effectively manage the infection.
In-Home Care
Home care is an essential part of the healing process for mild instances of walking pneumonia. Drinking enough water is essential since it thins mucus and promotes general health. Patients should consume a lot of water, herbal teas, or broths to stay hydrated. Rest is just as important; letting the body rest may greatly speed up the healing process.
Using humidifiers to keep the air moist can help control symptoms at home by relieving inflamed airways and easing breathing issues. In order to strengthen the immune system, patients should also pay attention to their food and eat a balanced diet full of vitamins and minerals. Applying a warm compress to the chest can help those who are uncomfortable with coughing-related chest pain.
Furthermore, it’s crucial to closely monitor symptoms. Patients should get medical help right away if their symptoms worsen or if they develop new ones, such as chest discomfort, a high temperature, or trouble breathing. This attention to detail can guarantee a speedy recovery and help avoid difficulties.
Possible Issues-Rising Walking Pneumonia Cases Explained
Even though walking pneumonia is usually mild and treatable, severe or untreated cases can have serious consequences. The emergence of secondary infections is one of the main dangers of walking pneumonia. The inflammation from the initial bout of pneumonia can make patients more susceptible to subsequent infections, such as bronchitis or even more severe types of pneumonia. For people who already have respiratory diseases like asthma or chronic obstructive pulmonary disease (COPD), this is especially troubling.
Additionally, severe or protracted walking pneumonia can lead to long-term disease or consequences, including pleurisy, an inflammation of the lung lining that can cause excruciating chest discomfort and breathing difficulties. Lung abscesses, which are pockets of pus that form in the lung tissue as a result of bacterial infection, can occur in rare cases. Significant morbidity may result from this illness, necessitating more intensive therapies such as surgery or protracted antibiotic regimens.
6. Strategies for Prevention-Rising Walking Pneumonia Cases Explained
Strategies for Prevention
Given the ongoing increase in walking pneumonia occurrences, it is critical to comprehend efficient preventative measures. Practicing personal and community-level precautions can significantly reduce exposure to respiratory diseases. This section explores practical measures that communities and people may take to reduce the risks of respiratory infections, like walking pneumonia.
Individual preventive actions
Proactive personal measures can significantly prevent walking pneumonia. Here are a few doable tactics to think about:
1. Hand hygiene:
Maintaining good hand hygiene is one of the best strategies to stop the spread of respiratory diseases. It’s crucial to regularly wash your hands with soap and water for at least 20 seconds, especially after using potentially contaminated surfaces or being in public. Using an alcohol-based hand sanitizer can be a useful substitute for soap and water if they are not accessible.
2. Wearing a mask can act as a barrier against respiratory droplets that could transport germs in crowded or poorly ventilated places. This is especially crucial when respiratory illnesses are common in the community or during flu season. Masks protect the wearer and others around them by lowering transmission.
3. Vaccination:
One essential preventive action is to stay current on your vaccines. We strongly advise the seasonal flu and pneumonia vaccines, as they can dramatically reduce the risk of respiratory infections. Vaccines strengthen the body’s defenses against illnesses and help prevent them from spreading. To find out which vaccinations are suitable for you and your family, speak with a healthcare professional.
4. Avoid Close Contact:
Keep people exhibiting signs of respiratory sickness at a distance. Steer clear of crowded areas where there is a greater chance of contacting infectious pathogens. You can reduce the transmission of pathogens by using social distance.
5. Practice respiratory etiquette:
When coughing or sneezing, cover your mouth and nose with a tissue or your elbow to promote proper respiratory hygiene. Throw away tissues right away, and then wash your hands. Following this simple procedure significantly reduces the risk of infecting others.
Prevention at the Community Level-Rising Walking Pneumonia Cases Explained
In order to stop the spread of walking pneumonia and other respiratory illnesses, community-level tactics are just as important as individual preventative measures. Schools, companies, and communities may adopt the following crucial practices:
1. Appropriate ventilation:
It’s critical to make sure interior areas have adequate ventilation. A healthy airflow lowers the danger of transmission by dispersing and diluting airborne germs. Maintaining HVAC systems, opening windows, and using air purifiers can enhance indoor air quality.
2. Sanitizing areas:
To stop the transmission of germs, it’s critical to routinely sanitize high-touch areas like light switches, doorknobs, and shared equipment. Implementing a regular cleaning program can significantly reduce the risk of respiratory infections in businesses and schools.
3. Promoting ill leave:
In order to stop epidemics in communities, it is crucial to encourage ill people to remain at home. By putting in place flexible sick leave policies, workers and students may take the time off they need to recuperate without worrying about losing their jobs or their grades. This procedure protects others from possible exposure in addition to the ill person.
4. Health Education Programs:
Workplaces and schools should provide educational materials that raise awareness of walking pneumonia and other respiratory diseases. People may learn about symptoms, preventative measures, and the value of getting medical help when needed from workshops and seminars.
5. Community vaccination drives:
Planning vaccination campaigns for the community may greatly raise immunization rates. Making vaccinations easily accessible can help safeguard susceptible groups and lower the prevalence of respiratory diseases in general.
The Function of Immunity-Rising Walking Pneumonia Cases Explained
Preventing respiratory infections, such as walking pneumonia, requires a robust immune system. People can improve their ability to fend off illnesses by concentrating on preserving and strengthening their immune systems. Here are some pointers for increasing immunity:
1. A balanced diet can help strengthen the immune system by consuming a range of fruits and vegetables that are high in vitamins and minerals. Antioxidants, zinc, vitamin C, and vitamin D are among the nutrients that are crucial for supporting the immunological response. Nuts, seeds, citrus fruits, and leafy greens should all be a regular component of one’s diet.
2. Frequent Exercise:
Regular physical exercise is beneficial for immune system function as well as general health. Exercise increases circulation, which facilitates the more effective passage of immune cells throughout the body. Try to get in at least 150 minutes a week of moderate-intensity activity, which might include swimming, cycling, or brisk walking.
3. Sufficient Sleep:
A strong immune system depends on getting enough adequate sleep. Sleep aids in infection prevention by allowing the body to heal and rejuvenate. Adults who want to maintain optimum immune function should strive for 7-9 hours of sleep each night.
4. Stress management:
Prolonged stress can weaken the immune system and increase a person’s vulnerability to illnesses. Including stress-reduction methods like yoga, meditation, mindfulness, or deep breathing exercises can boost immunological resilience and general well-being.
5. Supplements:
While a balanced diet should provide the majority of essential nutrients, some individuals may find it beneficial to take dietary supplements. It’s crucial to speak with a healthcare professional before beginning any supplements to be sure they are safe and suitable for your unique medical requirements.

7. Public health consequences-Rising Walking Pneumonia Cases Explained
Healthcare systems across the United States face serious issues as a result of the recent increase in respiratory diseases, especially walking pneumonia. Mycoplasma pneumoniae, the bacterium that causes walking pneumonia, has significantly increased in cases, particularly among young children, according to the Centers for Disease Control and Prevention (CDC). This strains pediatric care centers, which are frequently on the front lines of managing respiratory infections, in addition to hospitals and clinics.
Healthcare institutions encounter difficulties allocating resources as they deal with rising patient populations. In order to handle an influx of patients, hospitals must make sure they have enough personnel, supplies, and treatment choices. Longer wait times for patients may result from the increase in cases, especially in emergency rooms where patients with severe symptoms may require urgent attention. Furthermore, the financial strain on healthcare systems may worsen, resulting in higher operating expenses and possible budgetary limitations that affect the standard of service.
Physical resources are only one aspect of the problem; increased demands on healthcare workers are also contributing to exhaustion. This circumstance may worsen staffing shortages that existed before the epidemic by lowering employee morale and increasing turnover among healthcare professionals. Consequently, the combination of an increasing patient load and a reduced worker capacity seriously threatens the quality of treatment for patients with walking pneumonia and other respiratory conditions.
Public Health Awareness’s Function
Despite these obstacles, raising public health awareness is essential to halting the development of respiratory illnesses like walking pneumonia. Raising awareness can result in early symptom recognition, which is essential for efficient case management. Walking pneumonia symptoms include low-grade fever, exhaustion, and a persistent cough. These symptoms are frequently minor or mistaken for other conditions. By raising awareness of these signs and encouraging people to seek medical help promptly, we can significantly curb the virus’s spread.
Collaborations with neighborhood health groups, educational campaigns, and community outreach programs can promote a greater awareness of respiratory health. These initiatives can motivate individuals to adopt preventive measures like frequent hand washing, remaining at home during illness, and receiving vaccinations against influenza and pneumonia. Schools and businesses should also put in place training programs to teach staff and children the value of identifying respiratory problems early.
Additionally, using social media and digital platforms to spread information may reach a larger audience. Educational articles, films, and infographics can demonstrate the significance of identifying symptoms and comprehending the dynamics of walking pneumonia transmission. We can all work together to lower the prevalence of walking pneumonia in our communities by creating an atmosphere where people feel empowered to make wise health decisions.
A Look at Policy-Rising Walking Pneumonia Cases Explained
We might consider a number of policy actions to successfully address the rising incidence of walking pneumonia. First and foremost, government funding is essential for studies on respiratory infections like Mycoplasma pneumoniae. In the end, improved research can lessen the strain on healthcare systems by producing better diagnostic instruments, therapeutic alternatives, and preventative measures.
Along with financing for research, more financial assistance for healthcare institutions may help them hire more medical personnel, making sure they are prepared to deal with spikes in patient volume. This may also entail funding educational initiatives to help medical professionals identify and manage respiratory illnesses, such as walking pneumonia.
Furthermore, it is crucial to create all-encompassing reaction plans for future spikes in respiratory illnesses. This entails setting precise guidelines for handling epidemics and facilitating communication between healthcare practitioners and public health organizations to guarantee a coordinated response. In order to ensure that medical institutions can efficiently handle patient care without becoming overburdened, emergency preparation plans should include resources for testing, treatment, and immunization delivery during epidemics.
Furthermore, preventative measures, including expanding access to immunizations and supporting community health programs, should be the main emphasis of public health policies. We can lessen the effects of respiratory diseases by funding preventative care, which will also lessen the burden on healthcare systems and the frequency of infections.
8. Conclusion and Important Lessons
Walking pneumonia has increased in recent months, especially among children. Mycoplasma pneumoniae, the primary cause of this type of pneumonia, may lead to misdiagnosis due to its modest symptoms. A persistent cough, low-grade fever, and tiredness make it simple to mistake for a cold or other respiratory ailment. However, current statistics indicate a significant rise in cases, underscoring the importance of this condition for public health. Walking pneumonia cases among 2–4-year-olds have grown from 1% to over 7%. Same with older kids. Medical facilities, particularly those specializing in pediatrics, are experiencing a significant overload. Increased patient loads lead to exhaustion and worse care. Early response requires understanding of walking pneumonia symptoms. Proper cleanliness and keeping sick youngsters home are necessary to control this infection.
Motivation-Rising Walking Pneumonia Cases Explained
Individuals and communities must be vigilant in light of the circumstances. Understanding the symptoms and dissemination of walking pneumonia can improve early detection and treatment. Community health programs that educate the public can help people protect their families. Daycares and schools must also teach parents and children about respiratory hygiene, such as immunizations and handwashing.
As we go through this tough time, we must remember that our actions affect public health. Teaching kids to wash their hands and cover their mouths when coughing can reduce transmission. These little, effective steps may build a healthy neighborhood.
An Appeal for Action
Finally, if you or a loved one has walking pneumonia, consult a doctor immediately. Prevention of consequences and infection spread is possible with early detection and treatment. Medical practitioners may advise on symptom management and provide antibiotics.
Additionally, community-level health practices are crucial. Educational seminars, immunization campaigns, and local health activities can boost our respiratory infection resistance. A culture of health awareness and responsibility can safeguard our communities and vulnerable populations, notably children, who are more prone to walking pneumonia.
In conclusion, the rise in walking pneumonia incidence presents numerous challenges, but it also offers opportunities for community engagement and awareness. Being watchful and informed helps reduce the impact of this illness. We can improve procedures, support each other, and make the environment safer by working together.



