Introduction:
Managing chronic illnesses and rising demand for digital health solutions
Sometimes referred to as long-term ailments, chronic illnesses include cancer, diabetes, heart disease, and chronic respiratory disorders. These diseases greatly affect a person’s daily life and well-being and require ongoing medical therapy. Chronic Disease Management Software-The main causes of death and disability worldwide are chronic diseases, which increase the already heavy demand on healthcare services. With more than 70% of all fatalities worldwide attributed to chronic diseases, the World Health Organization (WHO) emphasizes the urgent necessity of efficient treatment plans.
Controlling chronic diseases in the past largely depended on in-person visits with medical experts, medication scheduling, dietary adjustments, and sickness course monitoring. But this approach is not always feasible, especially in rural or underdeveloped regions, and it usually produces divided treatment. Managing chronic illnesses (CDM) also requires constant, group efforts by patients, caregivers, and medical professionals. As such, digital health solutions meant to increase CDM’s efficacy, accessibility, and customization have proliferated.
Digital Health Solutions of CDM
Chronic Disease Management (CDM) software is one digital health tool that has revolutionized both patients and medical professionals in equal measure. Long-term sick individuals use these software programs to monitor, manage, and improve their care. Many times, CDM systems have several capabilities, including patient education, treatment tracking, real-time data collection, patient monitoring, and physician correspondence. These tools enable medical practitioners to offer more efficient and customized therapy, as well as allow individuals to actively participate in their health management.
CDM:
One of the key advantages of CDM software is its capacity to remotely monitor patients, therefore reducing the need for frequent hospital visits and allowing constant, real-time data collection. This is extremely useful in the management of disorders such as diabetes, hypertension, and heart disease, where it is imperative to carefully check blood pressure, blood sugar, and other important indicators. Linking wearable devices to CDM systems enables them to gather these parameters and notify medical specialists of any anomalies, allowing for quicker treatments.
Customized care plans are another tool in CDM systems that meet individual needs. This helps to assess adherence to meal recommendations, treatment plans, and prescription schedules. Software applications, for example, can remind patients to exercise or take their prescriptions on time, improving adherence and helping to reduce the issues resulting from non-compliance.

Benefits to Healthcare Systems and Patients
For those with chronic conditions, software for controlling them has several benefits. First of all, it encourages more involvement in self-health management—a habit that regularly yields better results. Access to educational resources, keeping in contact with support groups, and tracking their development over time help patients make wise medical decisions. Moreover, these systems usually provide direct channels of contact between patients and doctors so that they may ask questions or talk about problems without scheduling an appointment.
CDM tools help healthcare facilities handle large patient groups with chronic conditions, easing their burden. By facilitating remote monitoring and early problem detection, healthcare professionals may potentially decrease the need for emergency treatment or hospitalization. This facilitates early intervention. This results in better patient outcomes as well as reduced healthcare costs—a critical consideration given the significant financial burden chronic diseases create.
CDM Software’s Prospects
As digital health technology develops, CDM program capabilities will most likely grow. Combining modern technologies like artificial intelligence (AI) and machine learning will enable more tailored therapies and help foresee the direction of illnesses. AI, for example, may identify trends in patient data right away and suggest tailored treatment changes to improve patient outcomes.
Furthermore, as value-based care models—where patient outcomes rather than the volume of services provided take precedence—CDM software will become more important. These strategies fit the ability to provide proactive, continuous, customized care, therefore improving patient happiness and perhaps reducing medical costs.
How are long-term disorders managed?
Long-term health problems, most of which develop gradually, can seriously affect a patient’s quality of life. People frequently refer to one systematic approach to managing chronic diseases—also known as CDM—as non-communicative illnesses (NCDs) or chronic diseases; these conditions include diabetes, heart disease, hypertension, asthma, and arthritis. Unlike acute diseases, which show up suddenly and are usually fleeting, chronic diseases continue for a year or more and call for ongoing medical attention or limits on a person’s daily activities.
Chronic disease costs are increasing.
Over the past few decades, various elements, including urbanization, aging populations, sedentary lifestyles, and poor diets, have clearly raised the incidence of chronic diseases. With cancer, diabetes, chronic respiratory problems, and cardiovascular diseases at the top of the list, the World Health Organization (WHO) estimates that non-communicable diseases (NCDs) account for around 71% of all deaths globally. Effective management is absolutely essential for improving patient outcomes, lowering the likelihood of complications, and thereby relieving the financial burden on healthcare systems, as most of these diseases are incurable.
In the medical field, controlling chronic illnesses is very important.
2. CDM significantly helps to lower the increasing load of chronic diseases, highlighting a few key areas.
1. Benefit of proper chronic disease management is that it can help people live longer, better lives, free from additional challenges. CDM initiatives aim to reduce illness progression, enhance treatment plans, and improve patients’ overall quality of life.
2. By minimizing hospital admissions, ER visits, and the demand for costly procedures, CDM helps to reduce the financial load on consumers and healthcare systems. Early-stage therapy and continuous monitoring help to treat chronic diseases, which is far less costly than handling issues that have escalated.
3. The development of individualized treatment plans that meet the particular needs of every patient is of significant importance to CDM. These programs typically involve dietary changes, frequent symptom monitoring, medication regimens, and sickness education.
4. A basic component of the CDM approach is patient empowerment—that is, motivating patients to actively engage in the management of their conditions. Given the required knowledge and self-management tools, patients may effectively monitor their symptoms, follow advised treatment programs, and make informed decisions about their care.
5. Involves preventing complications from diseases: Poor management of chronic diseases can lead to serious adverse effects such as heart attacks, strokes, renal failure, and even death. By lowering the possibility of complications, proactive care of these diseases helps patients to lead better lives.
The Basics of Managing Chronic Illness
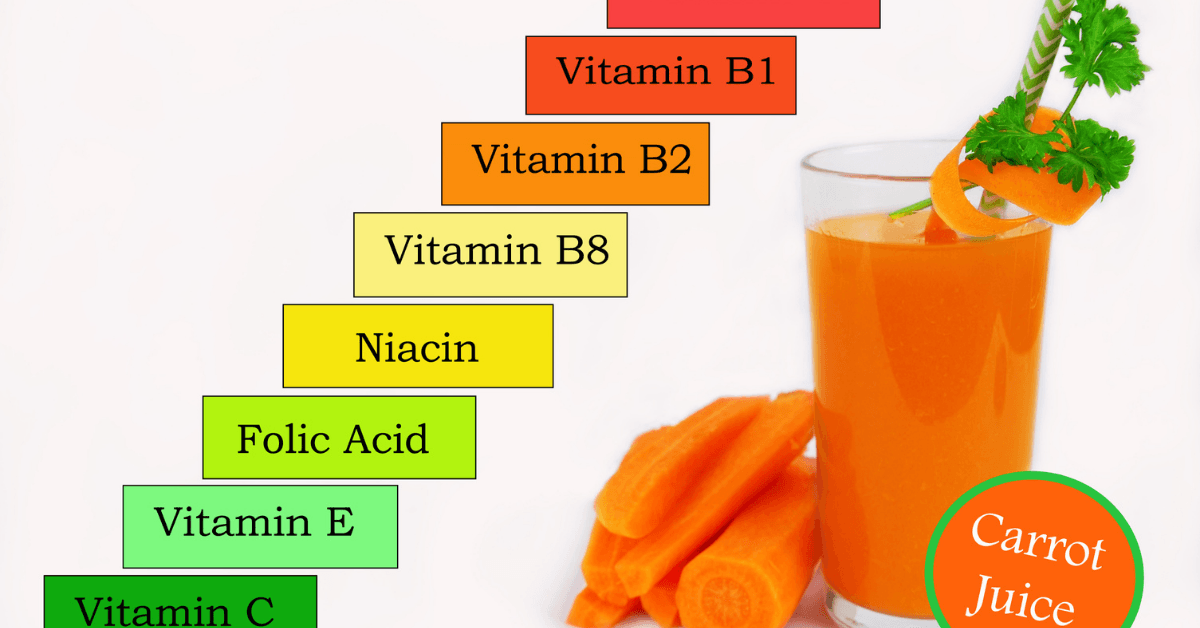
1. Education is a basic need of CDM, as patients have to understand their disease and how to manage it. This means knowing the possible effects of their illness, treatment, lifestyle changes, and symptom observation.
2. Treating chronic diseases usually calls for the knowledge and expertise of several healthcare experts, including doctors, nurses, nutritionists, and chemists. It entails coordinating treatment among multiple experts to ensure patients receive comprehensive and well-rounded care.
3. Technology Use:
Digital health resources play a crucial role in chronic disease management. With smartphone apps, wearable technologies, telemedicine platforms, and remote monitoring devices, patients and healthcare professionals may real-time track vital signs, medication adherence, and other health data. These technologies provide medical personnel with the knowledge they need to change treatment plans as needed and give individuals more control over their illnesses.
4. A key component of CDM is helping patients to acquire healthy habits like regular exercise, a balanced diet, stopping smoking, and stress management. These lifestyle modifications can greatly slow down the course of chronic diseases and enhance general well-being.
5. Medication management is crucial if one is to control chronic conditions. Making sure patients follow their medicines as advised, avoid harmful drug interactions, and appropriately control any side effects is absolutely essential for CDM. Healthcare professionals play a crucial role in evaluating and modifying a patient’s medication schedule based on their progress and any emerging issues.
6. Treatment of chronic diseases requires regular monitoring of important indications and symptoms. Those with long-term medical conditions usually monitor their development using blood pressure, blood sugar, cholesterol, and weight control. This helps to see any early signs of deteriorating health and guarantees quick response.
Common chronic diseases and their management
1. Diabetes is a condition whereby the body cannot effectively regulate blood sugar levels. Insulin resistance causes type 2 diabetes, while a lack of insulin production causes type 1 diabetes. Usually, controlling diabetes calls for regular blood glucose tests, lifestyle changes, and medication—such as insulin or oral hypoglycemics. Among other concerns, uncontrolled diabetes can lead to heart disease, kidney failure, and nerve damage.
2. Often called high blood pressure, hypertension increases the risk of renal failure, heart attack, and stroke. Apart from using medications like diuretics, ACE inhibitors, or beta-blockers, controlling hypertension also requires changing lifestyle choices, including reducing salt, maintaining a healthy weight, and increasing physical exercise.
3. Among the cardiovascular disorders are arrhythmias, heart failure, and coronary artery disease—all connected to the heart.
The CDM stresses medication management, lifestyle modifications, blood pressure, and cholesterol monitoring for chronic diseases. Frequently included in the treatment strategy are cardiac rehabilitation programs intended to improve heart condition and prevent further harm.
4. Asthma and chronic obstructive pulmonary disease (COPD) require ongoing care to minimize flare-ups and preserve lung function. To control symptoms, minimize triggers, and improve breathing ability, patients with asthma or COPD often use inhalers and other medications. For respiratory conditions, CDM’s key components include pulmonary rehabilitation and lifestyle changes, including smoking cessation.
5. Arthritis:
Especially rheumatoid arthritis and osteoarthritis—causes inflammation and ongoing joint pain. Among treatment strategies are painkillers, anti-inflammatory drugs, and physical therapy. Sometimes surgery is required in specific situations. Patients often recommend maintaining a healthy weight and engaging in low-impact exercises to reduce joint stress.
Treating chronic diseases requires the invaluable assistance of medical professionals.
Healthcare professionals mostly determine the success of CDM programs. Among their roles are:
Early identification and ongoing monitoring are prerequisites for CDM to effectively control symptoms and stop the disease from spreading.
Patient Education:
Providers inform patients about their ailments, available therapies, and self-management strategies, thereby arming them with the skills they need to control their own health.
Coordinating care: Providers team with a group of medical experts to ensure the patient receives complete therapy. This category includes prescription writing, problem handling, and, if needed, transferring patients to professionals.
Changing Treatment Plans: Regular evaluation and modification of treatment plans depending on patient response to medicine, any adverse effects, and any new symptoms is crucial as chronic diseases change with time.
3. Value of software for managing chronic diseases (CDM)-Chronic Disease Management Software
The World Health Organization estimates that chronic diseases—including diabetes, heart disease, and respiratory problems—account for 71% of all deaths globally, thereby ranking as the main cause of death. Managing these chronic health problems presents significant challenges for both people and medical institutions. A fresh approach to address these problems is software for chronic disease management (CDM), which makes improved medication adherence, continuous monitoring, and patient interaction using technology possible. Since CDM software directly improves patient outcomes, reduces expenses, and raises the overall general efficacy of healthcare systems, it is difficult to overestimate its relevance. Emphasizing the use of technology to manage chronic diseases, improve patient outcomes, and save healthcare costs, this article will investigate the critical role CDM software performs in transforming the management of chronic diseases.
1.The growing expense of chronic diseases
Chronic conditions contribute significantly to medical expenses. Chronic conditions account for 90% of the $4.1 trillion in annual healthcare spending in the United States. Because it gives acute care top priority over prevention and continuous maintenance, the conventional healthcare model sometimes fails in managing these complicated long-term diseases. By providing tools for continuous monitoring and therapy, software for managing chronic diseases seeks to address this disparity. This proactive strategy is absolutely vital for patients with chronic diseases to stop their condition from progressing, prevent complications, and finally improve their quality of life
2. Managing chronic diseases using technology
Thanks in large part to technical developments—particularly in the healthcare sector—the management of chronic conditions has greatly improved. Digital tools include wearables, telemedicine, mobile health apps, and electronic health records (EHRs) included with CDM software help to improve patient care. Thanks to these technologies, which provide real-time patient health status data, healthcare providers may make informed decisions and administer early therapies.
For instance, wearable gadgets tracking blood pressure, heart rate, and glucose levels constantly feed data to the program. When a patient’s condition deteriorates, the application subsequently alerts the staff in healthcare facilities. Early warning systems help prevent hospital stays and major effects by allowing interventions before the patient’s health deteriorates. Moreover, these technologies give patients the means to monitor their ailments and keep updated on their development, enabling them to actively control their health
3. Using CDM tools to maximize patient outcomes
The primary goal of CDM tools is to improve patient outcomes. Several elements improve patient education, treatment plan adherence, and coordination of care.
Care coordination:
CDM systems help professionals, caregivers, and medical providers to easily interact. This ensures that patients get consistent therapy, helps to eliminate unnecessary treatments, and reduces the likelihood of medical errors. EHR integration into CDM systems helps to share patient data required for thorough care planning
Treatment non-adherence is one of the main challenges to managing chronic illnesses. In order to handle this, CDM tools employ mobile apps to give patients tailored medication reminders, appointment alerts, and advice for lifestyle changes. These characteristics reduce the risk of hospital readmissions and illness progression by encouraging patients to follow their treatment plans
To help improve outcomes, arm patients with knowledge about their disease. Using CDM software, patients may access educational resources to increase their knowledge of managing their disease. Patients are encouraged to follow their treatment regimens, lead a healthy lifestyle, and frequently monitor their health in order to improve their self-management
4. Reducing medical expenses by employing CDM software
Although chronic diseases can tax healthcare systems financially, CDM software offers a reasonably priced solution. Through early treatments and avoidance of expensive hospital stays, CDM software can help healthcare providers reduce overall costs. In the following key ways, CDM software reduces expenses:
Using real-time alerts and monitoring helps doctors save expensive ER visits and hospital stays by acting before a patient’s health gets worse. For example, the system may alert a diabetic patient if their blood glucose level rises alarmingly and let them change their insulin dosage before problems start
Reducing Rehospitalizations:
Chronic diseases, particularly heart failure and COPD, often lead to rehospitalizations. Rehospitalization lessens when CDM systems track patient progress and guarantee adherence to treatment plans upon release. Automating administrative tasks, including patient data and appointment scheduling, saves time and money on handwritten procedures. This increases operational efficiency and reduces staff expenses by allowing medical professionals to focus on patient care rather than documentation
Enhanced Medication Management: CDM systems frequently have features to help patients better control their prescription regimens, thereby preventing expensive side effects resulting from mismanaged or missed dosages
Using CDM tools to improve preventative care
Preventive care is part of the management of chronic illnesses; therefore, CDM software is absolutely essential to move this approach forward. By utilizing predictive analytics and data insights, CDM software can identify those who are at risk of developing chronic diseases and implement preventive measures. Mobile health apps, for example, may offer tailored food and activity recommendations for those at risk of diabetes, thereby helping them to postpone the start of the illness. Moreover, telemedicine guarantees that patients maintain their health even in the absence of symptoms by allowing regular check-ins with medical experts

4. Key Components of Software Designed for Management of Chronic Illnesses (CDM)
Software for chronic disease management, or CDM, helps doctors treat patients with conditions including asthma, heart disease, diabetes, and hypertension. Many diseases need timely medical treatments, lifestyle changes, and continuous monitoring. As the sector moves to a more patient-centric and data-driven approach, CDM software has grown to be a vital tool for improving patient outcomes and saving healthcare expenditures. This paper will discuss the primary purposes of CDM software, which include drug adherence, care coordination, data analytics, telemedicine integration, patient monitoring, and more.
1. Patient monitoring
Patient monitoring is the CDM program’s most important use. Medical personnel may real-time monitor a patient’s vital signs, symptoms, and general condition with this technology. Wearables, glucometers, and heart monitors can sync with the software to deliver continuous data, therefore relieving patients of their need to routinely visit clinics. Remote monitoring helps to avert repercussions by identifying early signs of deterioration and allowing for quick action. Apart from enhancing the quality of service, constant patient monitoring increases patient involvement levels as people participate more actively in their own health care.
Monitoring also helps to create customized care plans, as data-driven insights allow doctors to change patient therapy depending on their current health condition. For diabetic individuals, for example, one may closely monitor their blood glucose levels and use the information to create alarms to adjust insulin doses. Real-time access to patient data helps healthcare professionals to make better decisions, thereby enhancing patient outcomes.
2. Telemedicine integration
Modern healthcare depends much on telemedicine, which is the foundation of CDM systems. Without having patients physically present at a facility, healthcare providers can interact with them by phone talks, internet chat, or video conferences. By relieving the burden on those living in remote areas or with mobility problems, telemedicine helps to make healthcare more accessible.
Telemedicine integration with CDM software simplifies patient-provider contact, ensuring quick consultations and follow-ups. Direct conversations regarding symptoms, treatment choices, and lifestyle changes between doctors and patients allow for Medical professionals can also remotely change treatment strategies. Those with chronic conditions who might not need frequent in-person visits but nevertheless require continuous treatment would especially benefit from virtual communication.
Furthermore, integrating telemedicine with CDM software ensures a comprehensive approach to disease treatment by allowing specialists to interact in real time about a patient’s condition, facilitating multidisciplinary cooperation. This improves the quality of treatment and reduces therapy delays.
3. Utilizing prediction models and data analytics
Data analytics is a strong tool that allows one to use patient data to enhance disease management. Examining prior medical records, present symptoms, lifestyle choices, and genetic data allows CDM software to identify trends that can predict possible health concerns. These predicted features let doctors intervene early to control problems before they become more serious.
For example, the application may project a heart attack risk and recommend preventative actions based on changes in a patient’s cholesterol or blood pressure. This function not only improves patient outcomes but also helps to cut healthcare expenses in general by lowering emergency hospitalizations.
Furthermore, data analytics enables doctors to evaluate the effectiveness of several treatment approaches, allowing for continuous improvement of patient care strategies. The initiative creates reports tracking patient development, treatment efficacy, and areas needing changes to care strategies. With this evidence-based approach, management of chronic diseases is definitely more exact and effective.
4. Coordinating Treatment
Care coordination is another essential element of CDM software that is particularly relevant for patients with complex medical needs. Treating chronic conditions usually calls for the cooperation of several healthcare providers, including therapists, nurses, specialists, and primary care doctors. Should the experts coordinate correctly, the patient will get consistent, integrated care.
By centralizing patient data and enabling communication across several healthcare workers, CDM tools help to simplify care coordination. All approved professionals engaged in patient care have access to current test findings, treatment plans, and health data. This ensures that everyone manages the patient’s health in agreement and lessens the risk of misinterpretation or uneven treatment.
Task management systems are another capability many care coordination technologies offer. These systems allow medical personnel to assign and track activities related to a patient’s care plan. For a follow-up test or a prescription change, for example, the system may immediately alert both the patient and the doctor.
5. Adherence to medications and management.
Managing a chronic condition and preventing patient difficulties depend on following a doctor’s prescription. Using notifications, reminders, and even treatment-related educational resources, CDM software aids in patient management of their prescription schedule.
Medication adherence tools remind patients when it is time for them to choose their prescriptions; the program lets doctors track adherence rates. If a patient often forgets their medications, the application may sound an alert, and medical experts might have time to intervene. Sometimes, the program goes so far as to suggest alternative medications when side effects or patient preferences compromise adherence issues.
Moreover, the medication management features of CDM software may communicate with pharmacies and electronic health records (EHRs) to guarantee the timely updating and renewal of prescriptions, thereby mitigating the risk of medication errors.
6. Patient engagement and education
In large part, treating chronic diseases depends on patient involvement. CDM software increases patient involvement by providing interactive tools, health advice, and educational resources to help patients better grasp and control their conditions. Active participants in their treatment are more likely to follow their goals, change their habits, and regularly contact their doctor.
Some CDM systems contain tailored training materials depending on the particular situation of the patient, such as diet advice for diabetes or exercise plans for heart diseases. These resources improve patient outcomes and compliance by empowering them to actively participate in their own treatment.
Common patient engagement tools, including symptom trackers, mood diaries, and lifestyle assessments, can provide patients with a whole picture of their health and inspire them to start active disease management programs.
7. Programs for Individualized Care
Not all chronic illnesses are manageable in every setting. Every patient’s circumstances are different and call for different care plans. Using CDM software, healthcare providers may create and modify treatment plans based on the evolving health needs of every patient. Medical experts can tailor plans to fit specific symptoms, patient preferences, and lifestyle.
Healthcare professionals can keep therapy responsive and relevant by making real-time changes to treatment plans based on patient input and monitoring data. For example, should a patient’s health either improve or worsen, the clinic can quickly adjust the treatment plan without calling a visit.
8. Integrating electronic health records (EHR)
To provide seamless patient treatment, CDM systems often interact with current Electronic Health Records (EHR) systems. Thanks to this link, medical personnel may now look at a patient’s full medical history, including past diagnosis, treatments, and test findings. By aggregating and making all patient data easily available, CDM software reduces the need for duplicate patient information by synchronizing with EHR systems.
EHR integration also simplifies care transitions for patients who are moving between many medical institutions or doctors, in particular. Having a single, thorough picture of the patient’s medical history helps healthcare professionals avoid reliance on erroneous or outdated knowledge while making decisions.
9. Supporting clinical decision-making
CDM systems commonly include clinical decision support (CDS) technologies, which assist medical professionals in making informed decisions about patient care. These instruments assess patient information and offer evidence-based recommendations for changes to therapy, medicine, and lifestyle.
A CDS system could recommend changing the dosage of medication according to recent lab results or extra testing. These instruments ensure that patients receive the best possible treatment by keeping healthcare workers up to date with the most recent clinical guidelines and research.
5. Advantages for Patients and Physicians: Better Treatment, Better Results, and Fewer Hospital Visits-Chronic Disease Management Software
Millions of people worldwide suffer from chronic illnesses such as diabetes, hypertension, heart disease, and chronic obstructive pulmonary disease (COPD), which places a heavy financial strain on healthcare systems. Programs for chronic disease management (CDM) and chronic care management (CCM) have shown to be useful strategies for addressing the difficulties brought on by these disorders. These initiatives improve healthcare outcomes, lower hospital readmission rates, and improve treatment quality for both patients and healthcare professionals.
Coordinated treatment strategies, individualized care plans, and thorough monitoring are the main components of managing chronic diseases. This framework helps patients take an active role in their health management by preventing the consequences of poorly treated or uncontrolled illnesses. This essay will examine how, by emphasizing better treatment, better health outcomes, and fewer hospitalizations, CCM and CDM programs benefit patients and providers alike.
1. Improved patient involvement and care
Chronic illness management empowers patients by providing them with the resources to self-monitor and participate in their treatment. Patients may track their symptoms, medication compliance, and general health status in real-time using digital health solutions like chronic illness management software, which helps them understand their condition better. Patients may also get food advice, health suggestions, and prescription reminders through these platforms to help them better manage their ailments on a daily basis.
This degree of participation significantly improves patient adherence to treatment programs when managing chronic diseases. For instance, diabetic patients can closely monitor their blood sugar levels, receive immediate feedback, and adjust their habits as necessary—all while maintaining constant communication with their healthcare professionals
2. Better health outcomes
Programs for managing chronic diseases assist individuals in preventing worsening of their symptoms through early detection and routine monitoring. Increased patient participation leads to a decrease in problems, which greatly improves overall health outcomes. Patients with hypertension, for instance, who routinely check their blood pressure are more likely to notice any aberrant readings early and take appropriate action, such as changing their lifestyle or medication.
Moreover, CDM programs give medical professionals access to actionable data, allowing them to conduct prompt treatments. Using digital platforms, healthcare professionals can respond more quickly to worsening illnesses by analyzing patterns in their patients’ health indicators. By slowing the advancement of chronic illnesses, this preventative strategy improves long-term results
3. Lower Hospital Expenses and Visits
Hospitalizations due to chronic disease complications account for a significant portion of healthcare expenses. Implementing chronic care management measures can significantly reduce the need for ER visits and hospital admissions. Research indicates that consistent observation and prompt therapies result in fewer flare-ups and acute episodes, helping patients avoid hospital stays altogether
This decrease in hospital visits results in cheaper operating expenses and more efficient use of resources for healthcare providers. Providers may focus on preventative care instead of reactive care, which involves treating patients when they are dangerously ill. This would lower the total economic load on healthcare systems. Preventive actions motivated by data and patient involvement result in better resource use and a decrease in avoidable hospitalizations
4. Improved provider-patient communication
For the treatment of chronic diseases, patients and healthcare professionals must communicate well. With the use of digital platforms made specifically for CCM, patients may communicate easily and report their symptoms and health indicators right away. By promptly offering suitable advice or modifying therapy, providers can avert issues and enhance patient outcomes.
Open communication strengthens the relationship between the patient and the provider, creating a more collaborative care environment. When patients feel encouraged by their medical staff, they are more likely to stick to their treatment regimens. Improved communication also enables physicians to address patient issues, provide information, and encourage patients, all of which lead to higher levels of patient satisfaction
5. Tailored Health Plans
The capacity to offer customized treatment plans is one of the main benefits of chronic illness management software. Individualized therapies are required to satisfy the specific requirements of patients with chronic illnesses. Healthcare professionals can use CDM systems to create personalized treatment plans by utilizing patient data such as health measurements, symptoms, and lifestyle variables.
These customized strategies raise patient compliance with care guidelines while also enhancing treatment efficacy. Patients’ greater commitment to adhering to the recommended regimen when they believe that their treatment regimens are tailored precisely for them leads to better results.
6. Improved patient satisfaction
For healthcare practitioners, patient happiness is a crucial indicator. Programs for managing chronic diseases increase satisfaction by providing convenience, improved health outcomes, and a more individualized approach to care. Patients benefit from proactive condition management, direct communication with their healthcare team, and easy access to their health data.
The sense of empowerment that comes from practicing self-management also contributes to increased patient satisfaction. Patients are happier with their healthcare when they can actively participate and control their health
7. Effective Utilization of Medical Resources
Programs for managing chronic diseases help healthcare professionals operate more efficiently and use resources more wisely. Reducing the number of emergency room visits and hospital stays allows healthcare facilities to concentrate on providing care for a larger patient population. Using technology, providers may monitor and communicate with patients remotely, allowing them to oversee greater patient populations.
This efficiency also applies to the distribution of resources and workers. Healthcare teams may devote more of their time to patient education, long-term planning, and preventative treatment rather than handling acute flare-ups
6. Software Types for Clinical Data Management (CDM)-Chronic Disease Management Software
Clinical data management (CDM) software is essential for managing the enormous quantity of data produced in healthcare, research, and medical trials. It ensures the precise, comprehensive, and verifiable gathering and updating of data for analysis, reporting, and regulatory compliance. Various CDM software types, including wearable device integration, patient self-management applications, and remote patient monitoring, cater to specific use cases. In this post, we will look at the various CDM software categories and discuss their implications for healthcare.
1. Platforms for Telemonitoring
Platforms for remote monitoring are a vital component of the CDM ecosystem. Medical professionals can monitor patients’ health information from a distance using these platforms, facilitating prompt interventions and ongoing care outside of a hospital. Remote monitoring solutions automatically input data into the system by gathering it from a variety of sources, including wearable technology, medical equipment, and patient-reported outcomes. This enables medical professionals to monitor a patient’s health from a distance and make data-driven choices.
For instance, while at home, a patient with heart disease can have their vital signs—blood pressure, heart rate, and oxygen levels—monitored. The healthcare practitioner receives the data instantly, making it possible to identify anomalies early on. Remote monitoring increases patient convenience, reduces the need for repeat hospital visits, and improves results by allowing early intervention.
Principal Elements of Platforms for Remote Monitoring:
A. Gathering data in real time from several sources
B. Integration with home monitoring systems and wearable technology
C. Constant monitoring for long-term diseases like diabetes or high blood pressure
D. Safe data transfer and storage to clinician portals or Electronic Health Records (EHRs)
In the context of managing chronic diseases, remote monitoring CDM systems are especially helpful in managing chronic diseases because continuous data gathering can reveal early indicators of decline and avert hospital admissions
2. Wearable device integration
Wearable technology has dramatically changed clinical data management and collection have changed dramatically as a result of wearable technology. These gadgets continually gather a variety of health data, such as heart rate, sleep patterns, and activity levels. Examples of these gadgets include smartwatches, fitness trackers, and health-focused wearables like ECG monitors. This data, when combined with CDM systems, offers a thorough picture of a patient’s health over time, improving diagnosis, care plans, and preventative measures.
Main advantages of including wearable technology:
A. Continuous Data Flow: Wearables continuously gather data without the need for patient involvement, giving analysts access to a smooth and comprehensive dataset.
B. Early Detection: By tracking vital signs and issuing warnings when thresholds are reached, wearables can identify early indicators of illnesses or exacerbations.
C. Patient Engagement: By giving patients access to real-time information about their own health parameters, wearables motivate patients to take a more active role in their care.
Integrating wearables with EHRs or CDM platforms provides physicians with comprehensive data that they can analyze alongside other health information, thereby enhancing the overall quality of treatment. A doctor can use activity data from a fitness tracker to determine a patient’s level of physical activity and modify treatment recommendations based on that information-Chronic Disease Management Software
3. Apps for Self-Management by Patients
Another crucial category of CDM software is self-management applications, which provide users the ability to take charge of their own health. These smartphone applications allow patients to monitor their symptoms, diet, exercise, and medication compliance. These applications help people manage chronic diseases, including diabetes, asthma, and hypertension, by offering goal-setting tools, prescription reminders, and instructional content.
For example, a hypertension control app can measure a user’s blood pressure, remind them to take their medication at prescribed times, and provide trend-based feedback. Additionally, it can provide food recommendations to lower blood pressure. Enhancing the patient’s self-efficacy can result in improved health outcomes.
Important self-management app features:
A. Symptom Tracking: Patients can log their symptoms and send them to medical professionals.
B. Medication Management: Apps frequently include reminders for taking prescriptions and adherence tracking.
C. Educational Resources: Patients receive educational resources, advice, and instructions to help them better understand their illness.
Some applications enable direct connections between patients and healthcare practitioners, facilitating consultations or emergency notifications.
Self-management applications give patients the resources they require to actively participate in their care. These applications are essential for people with long-term diseases like diabetes because they monitor blood glucose levels and assist with diet and insulin administration-Chronic Disease Management Software
4. Apps for Medication Management
Medication management applications, sometimes included in more comprehensive CDM software, assist patients in managing their prescriptions. By helping patients take the proper amount at the appropriate time, these applications help prevent mistakes in medicine administration. This is especially important for older patients or those who take multiple medications, because the complexity of drug management may result in errors or non-adherence.
Important Medication Management App Features:
A. Pill Reminders: These provide timely reminders for every dosage, lowering the possibility of missing or misplaced pills.
B. Medication refill alerts: notifications about a medication’s expiration date.
C. Interaction Warnings: Notifications sent when a new drug interacts with an already prescribed one.
Apps for medication management increase patient compliance and lower the risk of problems caused by missing or incorrectly administered doses. These technologies also assist healthcare practitioners by providing information about the patient’s adherence to recommended medicines, enabling modifications as needed
5. Systems for Electronic Data Capture (EDC)
EDCs, or electronic data capture systems, enhance the efficiency of data collection in research and clinical trials. They ensure the electronic recording of data, thereby reducing the likelihood of errors and enhancing data precision. Researchers can gather and analyze data more effectively thanks to these tools, which take the role of paper-based data input.
EDC systems frequently include the following characteristics:
A. Real-time data entry: Researchers can enter information as soon as they see a patient thanks to this feature.
B. Validation checks: making sure the entered data is accurate and satisfies predetermined standards.
C. Audit trails: monitoring data modifications for openness and adherence to legal requirements.
EDC systems play a critical role in clinical trials by guaranteeing that all data gathered is standardized and suitable for submission to regulatory bodies
7. Difficulties and Restrictions
The use of technologies like cloud computing, telemedicine, the Internet of Healthcare Things (IoHT), and Electronic Health Records (EHR) is causing a digital revolution in the healthcare industry. We expect these developments to reduce costs, improve patient outcomes, and boost healthcare efficiency. However, these developments also present significant obstacles. Patient compliance, system integration, and data protection are three major challenges that healthcare companies must deal with. To fully achieve the promise of digital health solutions, each of them creates obstacles to the smooth functioning and usage of healthcare technology. The restrictions must be overcome.
Concerns Regarding Data Privacy
Data privacy is a top priority for the healthcare industry because it handles extremely sensitive personal data. The digitalization of healthcare data and its storage in cloud systems or Internet of Health Technologies devices increases the risk of data breaches, illegal access, and privacy violations. Laws such as the General Data Protection Regulation (GDPR) in Europe and the Health Insurance Portability and Accountability Act (HIPAA) in the United States further mandate healthcare providers’ moral and legal duty to protect patient data-Chronic Disease Management Software
Difficulties with data privacy:
A. Unauthorized Access and Breaches:
Cyberattacks that target healthcare systems, such as phishing and ransomware, pose serious risks. These assaults may endanger both patients and healthcare organizations, resulting in unauthorized access to medical information. Maintaining real-time monitoring and making sure that only authorized individuals have access to sensitive data are significant challenges. The lack of infrastructure to safeguard enormous volumes of digital health data frequently exposes healthcare companies to breaches
B. Complexity of Compliance:
Healthcare providers need to adhere to a number of privacy laws, which differ depending on the location. This complexity further burdens healthcare companies, especially when data spreads across multiple platforms and legal countries. Failure to meet these requirements could result in severe fines and damage to a company’s reputation.
C. Data Sharing Dilemmas:
In order to conduct research, move patients between institutions, and coordinate treatment efforts, healthcare organizations must exchange data. This increases the likelihood of privacy breaches, particularly in the event that different firms use different security procedures-Chronic Disease Management Software
Resolutions:
a. To guarantee the confidentiality of sensitive patient data, multi-factor authentication (MFA), secure IoHT devices, and modern encryption techniques are important. Furthermore, conducting frequent audits, educating employees about data security best practices, and upholding stringent access limits can reduce privacy concerns
Combining Healthcare Systems with Integration
The integration of different systems and technology is one of the biggest challenges facing the healthcare industry today. In order to provide patients with comprehensive and well-coordinated treatment, it is imperative to establish a single system in which various platforms, databases, and apps may interact with one another.
Difficulties with system integration
a. Interoperability Problems:
A lot of healthcare facilities employ different systems, which makes communication and data exchange difficult. The incompatibility of EHR systems from various manufacturers, for instance, might make it challenging for medical practitioners to obtain a patient’s whole medical history. The integration of various systems may need costly and time-consuming proprietary solutions in the absence of a common communication protocol
b. Data fragmentation:
Dispersed patient data due to poor integration hinders provider collaboration. This may result in mistakes, unnecessary testing, and ineffective treatment, all of which would eventually drive up costs for patients and providers alike. Moreover, fragmented data hinders the development of customized treatment by making it more difficult to draw conclusions from patient data
c. Legacy Systems:
A lot of healthcare institutions still use antiquated technology, which makes it challenging to interface with newer systems. Updating or replacing these systems comes at a high expense, potentially affecting service delivery. Furthermore, healthcare personnel who may not be conversant with newer technology frequently oppose the process of switching from older systems to more modern, integrated ones
Resolutions:
a. Adopting industry-wide standards such as Fast Healthcare Interoperability Resources (FHIR) and Health Level 7 (HL7) can enhance system interoperability and streamline the sharing and interpretation of healthcare data. Furthermore, implementing scalable and flexible cloud-based solutions can help close the gap between heterogeneous systems, facilitating more seamless integration without completely replacing traditional systems-Chronic Disease Management Software
Patient Involvement
Patient compliance continues to be a behavioral and social issue that impacts the effectiveness of healthcare delivery, even while data privacy and system integration represent substantial technological obstacles. We refer to compliance as the degree to which patients adhere to advised lifestyle modifications, follow-up appointments, and prescription medicines.
Obstacles to patient compliance:
a. Complicated Treatment Plans:
Individuals with long-term illnesses frequently need to follow intricate, multi-drug regimens and adjust their lifestyles, which can be challenging to follow. Noncompliance with these strategies may lead to worse health outcomes, readmissions, and higher medical expenses. Furthermore, patients may have poor compliance due to forgetting to take their meds or not completely understanding their treatment plan.
b. Social and financial barriers:
Cost is a major barrier preventing many patients from following their treatment programs. Financial hardship may result from regular check-ups, therapy, and medication, particularly for individuals who are underinsured or without insurance. Social variables, including the absence of encouragement from friends or family, might also contribute to non-compliance.
c. Technology-Related Compliance:
Some patients, particularly the older people or those with limited digital literacy, find it difficult to accept new technology as healthcare moves toward telemedicine and digital health platforms. These people might not use healthcare apps, which could result in missed appointments, sluggish communication, or incorrect medication administration
Resolutions:
a. By providing timely medication and appointment alerts, mobile health (mHealth) solutions and reminders via apps can improve patient compliance. Healthcare practitioners can also use less complicated means of communication, including phone calls or SMS-based reminders, to connect with older patients or others who are not as tech-savvy.
Enhancing compliance can also involve addressing financial obstacles with more open pricing, financial aid plans, and unambiguous information about the long-term advantages of adhering to the plan.
8. CDM Software’s Future
Globally, chronic illnesses, including diabetes, heart disease, and respiratory disorders, are among the main causes of death and disability. As these disorders become more common, effective chronic disease management (CDM) strategies become more and more necessary. In the past, patient education, medication adherence, and routine checkups have been the mainstays of CDM. However, this environment is fast changing due to technological breakthroughs. CDM software, with its advanced features such as wearable technology, predictive analytics, and AI integration, is revolutionizing the tracking and treatment of chronic illnesses.
This essay will examine how these new developments are influencing CDM software going forward, and how they may be able to improve patient care, lower medical expenses, and provide better results.
1. AI integration: revolutionizing CDM
In healthcare innovation, artificial intelligence (AI) is leading the way, especially when it comes to managing chronic diseases. AI algorithms can analyze large datasets such as genetic profiles, patient histories, and real-time data from wearables to identify trends and predict the progression of disease. AI integration with CDM software can support ongoing monitoring, individualized treatment regimens, and early problem detection.
a) AI-Powered Customized Care
AI-powered CDM software, which analyzes patient data to suggest targeted actions, can provide personalized care. AI, for instance, is capable of autonomously adjusting insulin doses based on an analysis of a patient’s blood glucose levels. This level of customization enhances patient outcomes by providing real-time adaptive care options.
b) Automating Daily Jobs
Healthcare practitioners may focus on more sophisticated care activities by using AI to automate mundane chores like data input, prescription reminders, and appointment scheduling. Automation increases the operating efficiency of healthcare institutions and reduces administrative hassles.
2. Prognostic Analysis for Disease Advancement
Predictive analytics is one of the most exciting uses of AI in CDM software. AI can predict the course of an illness by analyzing patient data, allowing for earlier intervention and better care. AI, for example, may analyze patient biometrics to forecast the risk of heart attacks or strokes, allowing for prompt medical intervention. Devices: Real-Time Monitoring and Data Collection
From basic fitness trackers to complex instruments that can continuously monitor a range of health markers, wearable technology has advanced. When combined with CDM software, these gadgets can offer insightful information on a patient’s condition, improving disease management and prevention.
a) Ongoing Health Assessment
Wearable technology, such as heart rate monitors, glucose monitors, and smartwatches, can continuously track a patient’s vitals. By feeding the information gathered from these sensors into CDM software, medical professionals may get real-time patient condition insights. This ongoing monitoring may be able to prevent chronic illnesses from getting worse by enabling prompt actions.
b) Disability empowers individuals by equipping them with the necessary resources to manage their own health. By monitoring their physical activity, sleep habits, and medication compliance, they may make better-informed decisions regarding their health and way of life. Patients with chronic illnesses can use wearable devices to connect with CDM software to track their progress and develop individualized health objectives.
b) Patient monitoring via remote access
Wearable technology not only empowers patients but also makes remote patient monitoring possible—a crucial component of telehealth. This saves time and money by lowering the need for frequent in-person medical appointments. Remote monitoring is especially helpful for patients who reside in underserved or rural locations since it guarantees ongoing treatment without requiring them to travel far.
3. Practice management via predictive analytics
AI-powered predictive analytics is another revolutionary development in the treatment of chronic illnesses. Based on past data, present patterns, and up-to-date medical knowledge, it enables healthcare professionals to forecast potential health hazards in the future. Including predictive analytics in CDM software transforms the management of chronic illnesses from reactive to proactive.
a) Early Health Complication Identification
The use of predictive analytics facilitates the timely identification of possible health issues before they worsen. Predictive analytics, for example, can anticipate hypo- or hyperglycemia episodes in diabetic patients, enabling prompt treatments to avoid emergencies. This enhances long-term health outcomes and reduces hospital admissions.
b) Tailored intervention strategies
Predictive analytics analysis can assist in developing individualized treatment regimens catered to the unique needs of each patient. This makes therapy suggestions and dose modifications more precise. Predictive algorithms, for instance, can examine past blood pressure data and food patterns to provide patients with hypertension with tailored diet recommendations.
c) Resource optimization and cost reduction
Predictive analytics in CDM software also has the potential to save healthcare expenses. Healthcare providers can save money on costly emergency treatment and hospital stays by anticipating health concerns and preventing complications. When managing chronic illnesses with a large patient load, resource optimization ensures hospitals don’t overburden themselves with unnecessary care or hospital stays.
4. Data-Informed Decision Making
The management of chronic diseases is becoming increasingly data-driven with the integration of wearable analytics and artificial intelligence. Real-time data and predictive insights enable healthcare practitioners to make well-informed decisions that improve patient outcomes and streamline the delivery of treatment.
a) Data integration and interoperability
Data interoperability is essential for CDM software to function as intended. One platform has to be able to easily combine data from many sources, such as patient self-reports, wearables, and electronic health records (EHRs). We are creating advanced CDM systems to facilitate interoperability. These systems will let healthcare practitioners view and evaluate a patient’s whole medical history in one location.
b) AI-Powered Healthcare Provider Insights
AI can provide healthcare practitioners with valuable insights by analyzing vast amounts of patient data. These insights enable healthcare practitioners to improve treatment plans, anticipate future consequences, and make informed decisions regarding a patient’s care. Thus, data-driven decision-making saves time and effort compared to human data analysis while also enhancing the quality of service.
9.Conclusion:
With its ability to provide vital tools for the efficient treatment of long-term health disorders, chronic disease management software, or CDMS, represents a significant achievement in the healthcare industry. Through meticulously recording and monitoring patients’ health data, these software solutions help healthcare professionals to enhance patient care. They also help to properly control treatment regimens and prescribed medicines. CDMS plays a significant role in improving communication among healthcare teams. This ensures that customized treatment is tailored to the specific needs of each patient.
CDMS:
The potential of chronic illness management software to promote proactive patient participation is one of its main advantages. Including tools like appointment scheduling and medication adherence reminders increases the likelihood of patients actively participating in their own care. This not only improves health outcomes, but also encourages greater adherence to treatment plans-Chronic Disease Management Software
Furthermore, healthcare practitioners may find significant value in the data gathered by CDMS. Examining patterns in patients’ health over time enables better decision-making. This allows medical professionals to modify treatment plans as needed, potentially avoiding problems caused by chronic illnesses.
Strong CDMS solutions are absolutely vital for hospitals. Particularly since the need for management of chronic diseases keeps rising, this investment improves care delivery and helps to minimize running expenses. CDMS improves patient outcomes by efficiently applying technology in healthcare. It also makes the system generally more sustainable and efficient at the same time. In the end, the incorporation of chronic disease management tools guarantees that patients with chronic conditions get the complete therapy they need.



